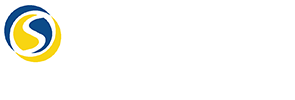
Insulin resistance is a metabolic condition where the body’s cells become less responsive to the effects of insulin. Normally, insulin facilitates the uptake of glucose into cells, thus maintaining balanced blood sugar levels. When cells resist insulin’s action, the pancreas compensates by producing more insulin, creating a cycle that can lead to elevated blood sugar and eventually, type 2 diabetes. This condition is often a precursor to various other health complications, emphasizing the need for early intervention.
Insulin resistance doesn’t develop overnight; it’s the result of a complex interplay of genetic, lifestyle, and dietary factors. A sedentary lifestyle, poor dietary choices, and inadequate sleep can accelerate its onset. Understanding these contributing factors is essential for preventing the condition and maintaining metabolic health. Addressing lifestyle elements, such as sleep, can be a pivotal step in reversing or managing insulin resistance.
How Sleep Affects Insulin Sensitivity
Research consistently underscores the strong link between sleep and insulin sensitivity. Adequate sleep is not merely a passive state of rest but a dynamic process where critical bodily functions, including metabolism and insulin regulation, are optimized. During sleep, the body carries out essential repairs and hormonal adjustments that are vital for maintaining insulin sensitivity and metabolic balance.
Moreover, during the various stages of sleep, the body regulates the production of hormones that influence hunger and glucose metabolism. This regulation ensures that insulin functions efficiently, preventing blood sugar spikes and maintaining overall metabolic health. Thus, sufficient sleep acts as a protective factor, enhancing the body’s ability to utilize insulin effectively and reducing the risk of insulin resistance.
Sleep Deprivation and Insulin Resistance
Lack of sleep, or sleep deprivation, poses a significant threat to insulin regulation. Even short-term sleep loss can disrupt the body’s ability to process insulin, leading to increased blood sugar levels. This impaired insulin function can set the stage for developing type 2 diabetes, especially if sleep deprivation becomes chronic. Therefore, ensuring adequate sleep is crucial for maintaining insulin sensitivity and preventing metabolic disorders.
The body perceives sleep deprivation as a form of stress, which triggers the release of stress hormones like cortisol. Elevated cortisol levels can further impair insulin sensitivity, exacerbating the risk of insulin resistance. This hormonal imbalance underscores the need for prioritizing quality sleep as part of a comprehensive approach to metabolic health and diabetes prevention.
The Impact of Poor Sleep on Blood Sugar
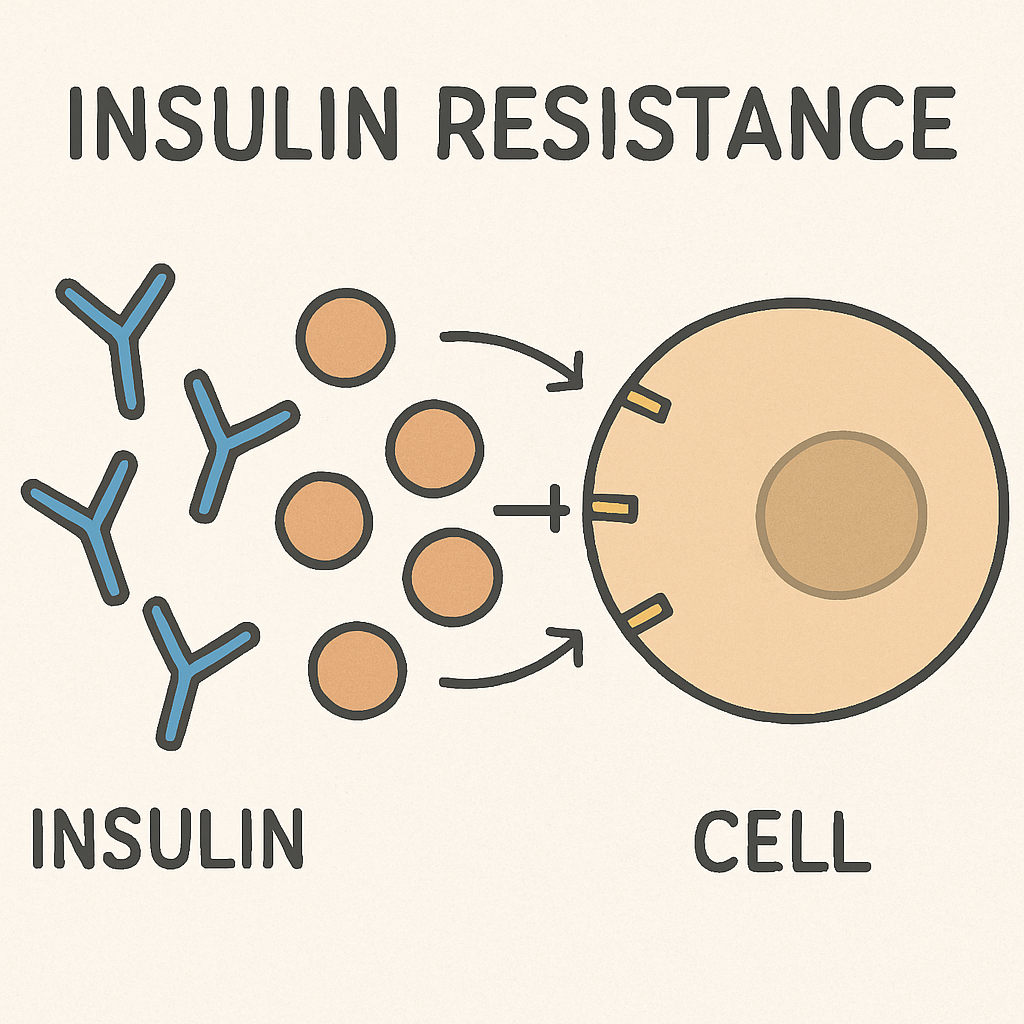
Poor sleep can disrupt blood sugar regulation, leading to unpredictable spikes. When the body lacks sufficient rest, it responds by releasing stress hormones like cortisol, which can elevate blood sugar levels. This physiological response creates a feedback loop where elevated blood sugar levels can further disrupt sleep, perpetuating the cycle of poor sleep and insulin resistance.
Beyond hormonal imbalances, poor sleep also affects the body’s circadian rhythms, which play a crucial role in glucose metabolism. Disrupted circadian rhythms can lead to misalignment in the body’s insulin production and glucose regulation, contributing to higher blood sugar levels. Addressing sleep quality is therefore integral to breaking this cycle and restoring balance to metabolic functions.
Sleep Disruption and Pancreatic Function
The pancreas, which is pivotal in insulin production, can be adversely affected by sleep disruption. Chronic sleep disturbances can impair the pancreas’s ability to produce and release insulin efficiently, leading to decreased insulin sensitivity. This inefficiency can push the body toward insulin resistance, highlighting the critical role that quality sleep plays in pancreatic health and overall metabolic function.
In addition to affecting insulin production, sleep disruption can alter the secretion of other hormones involved in glucose metabolism. This hormonal imbalance can further strain the pancreas, making it harder for the body to maintain normal blood sugar levels. Ensuring restorative sleep can help protect pancreatic function and support metabolic health.
Bedtime Routines for Glucose Control
Establishing a healthy bedtime routine can have a profound impact on sleep quality and blood sugar regulation. A structured routine signals the body that it’s time to wind down, promoting better sleep and, consequently, improved glucose control. Implementing these habits can be an effective strategy in managing insulin sensitivity and reducing the risk of type 2 diabetes.
Consistent Sleep Schedule
Maintaining a consistent sleep schedule by going to bed and waking up at the same time every day helps regulate your body’s internal clock. This consistency enhances sleep quality and supports the body’s ability to manage insulin effectively. By synchronizing your sleep patterns with your biological rhythms, you can improve overall metabolic health and reduce the risk of insulin resistance.
Consistency in sleep patterns also enhances the body’s circadian rhythm, which plays a critical role in hormone regulation, including those involved in glucose metabolism. By adhering to a regular sleep schedule, you optimize these hormonal cycles, supporting better insulin sensitivity and glucose regulation.
Sleep-Friendly Environment
Creating a sleep-friendly environment is vital for enhancing sleep quality. Keep your bedroom cool, dark, and quiet to minimize disturbances that can interfere with restful sleep. Using blackout curtains and white noise machines can help create an ideal sleep setting. Additionally, investing in a comfortable mattress and pillow can further improve sleep quality, making it easier for the body to regulate insulin and maintain blood sugar balance.
A sleep-conducive environment also involves minimizing potential sleep disruptors, such as electronic devices and ambient light. By eliminating these distractions, you promote deeper, more restorative sleep, which is essential for optimal insulin function and metabolic health.
Limit Caffeine and Screen Time
Avoiding caffeine and electronic screens at least an hour before bedtime is crucial for promoting restful sleep. Caffeine is a stimulant that can hinder your ability to fall asleep, while the blue light emitted by screens can disrupt your body’s natural sleep-wake cycle. By limiting these factors, you support your body’s ability to enter a restful state, enhancing insulin sensitivity and reducing the risk of insulin resistance.
Reducing screen time before bed also minimizes exposure to artificial light, which can interfere with the production of melatonin, the hormone responsible for regulating sleep. By fostering a calming pre-sleep routine, you create an environment conducive to quality sleep and improved metabolic health.
Improving Sleep to Prevent Diabetes

by Slaapwijsheid.nl (https://unsplash.com/@slaapwijsheid)
Improving sleep quality is a powerful tool in the fight against insulin resistance and type 2 diabetes. Prioritizing sleep as part of your wellness routine can significantly enhance insulin sensitivity and reduce the risk of metabolic disorders. By adopting strategies to improve sleep, you can take proactive steps toward better health and diabetes prevention.
Prioritize Sleep
Recognizing the importance of sleep and making it a priority in your daily routine is essential for supporting insulin function. Aim for 7-9 hours of quality sleep each night to optimize your body’s ability to regulate insulin and maintain stable blood sugar levels. Prioritizing sleep not only contributes to metabolic health but also enhances overall well-being.
Beyond mere quantity, focusing on the quality of sleep is crucial. Ensuring uninterrupted, restorative sleep allows the body to perform essential functions that support insulin sensitivity and glucose metabolism. By valuing and prioritizing sleep, you lay the foundation for improved metabolic health.
Manage Stress
Stress management is a critical component of improving sleep quality and insulin sensitivity. Chronic stress can negatively impact sleep and disrupt hormonal balance, leading to impaired insulin function. Engaging in stress-reducing activities like yoga, meditation, or deep breathing exercises can enhance sleep quality and help lower blood sugar levels, supporting metabolic health.
Incorporating stress management techniques into your daily routine not only improves sleep but also promotes a more balanced hormonal environment, reducing the risk of insulin resistance. By addressing stress, you create a more conducive environment for restorative sleep and optimal metabolic function.
Regular Physical Activity
Regular physical activity is a cornerstone of both sleep quality and insulin sensitivity. Engaging in at least 150 minutes of moderate exercise each week can significantly enhance sleep and improve insulin function. However, it’s important to avoid vigorous exercise close to bedtime, as it may interfere with sleep.
Exercise not only promotes better sleep but also enhances the body’s ability to utilize insulin effectively, reducing the risk of insulin resistance. By integrating physical activity into your routine, you support both sleep and metabolic health, contributing to a lower risk of type 2 diabetes.
Conclusion
Sleep is an often-overlooked factor in managing insulin resistance and preventing type 2 diabetes. By understanding the connection between sleep and insulin sensitivity, you can take proactive steps to improve your sleep and safeguard your health. Implementing healthy sleep habits and managing stress can significantly reduce your risk of insulin resistance and contribute to overall well-being. Remember, prioritizing sleep is not just about feeling rested; it’s about maintaining a healthy balance in your body’s functions, including insulin regulation. By taking control of your sleep, you’re also taking control of your health.
Understanding the profound impact of sleep on metabolic health highlights the importance of integrating sleep into a comprehensive approach to diabetes prevention. By fostering an environment that promotes quality sleep and addressing lifestyle factors that influence sleep, you can significantly enhance your body’s ability to manage insulin and maintain metabolic equilibrium. In doing so, you not only protect against insulin resistance but also improve your overall quality of life and long-term health prospects.